Can a gluten-free diet exacerbate a pre-existing brain condition? Changes in your diet can alter your microbiome within 1-2 days. When you remove wheat from your diet (which is a good thing to do), you remove the ‘bad guys’ in wheat that cause inflammation in every human. But you also remove the ‘good guys’ in wheat (called prebiotics) that starve the good bacteria in your gut. This will then cause more inflammation in your gut, contributing to the leaky gut, which opens the gateway in the development of autoimmune diseases (thyroid, brain, heart, skin, joint,…).
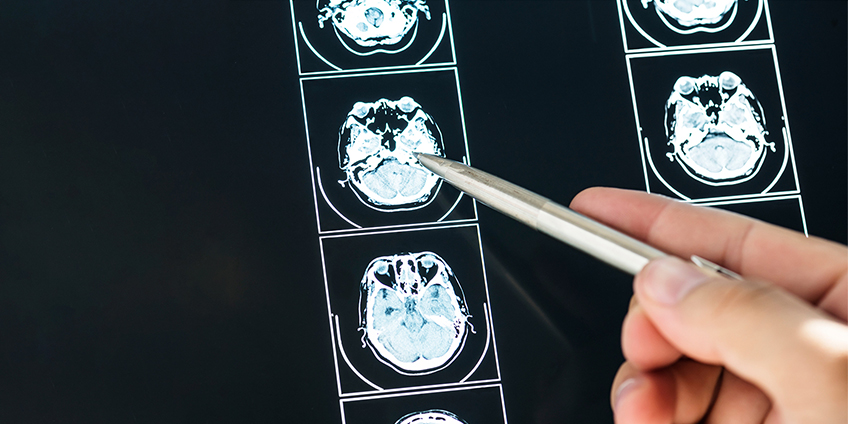
How Does Your Gut Health Impact Your Brain Health?
Research has indicated that a very strong gut-brain axis exists, and it has bi-directional communication. For every one message from the brain to the gut, there are nine messages from the gut to the brain. Therefore, it should come as no surprise that when you have problems in your gut, they could include medical concerns of a neurological nature. Your gut controls brain function. Ever heard of “going with your gut?” Many people refer to the gut as your “second brain.” Personally, when you read the science, I would say there’s a good argument that the microbiome in your gut is the ‘Command Center’ of your brain. It has its hands on the steering wheel of which direction your brain is going.
There is a recognized association between celiac disease and other gluten-related disorders with conditions in the fields of behavioral and mental health, as well as neurocognitive disorders.
This spectrum includes the following:
- Anxiety
- Dysthymia
- Depression
- Attention-deficit Hyperactive Disorders
- Mood and Sleep Disorders
- Mal Social Adaptation
- Substance-related
- Addictive and Neurocognitive Disorders
- Suicide
- Learning Disabilities
- Feeding and Eating Disorders
- Bipolar Syndromes
- Schizophrenia
- Autistic Spectrum Disorders
Treatment for celiac disease and other gluten-related disorders involves strict adherence to a gluten-free diet. For people with one or more of these conditions listed above, it is particularly important not to further inflame an already chronic medical condition. It just makes sense to check and see if gluten is a problem for you.
Start with the Gut
Probiotics are beneficial bacteria that vary in strains, each strain carrying with it specific properties that support health in its own unique way. Prebiotics are the foods probiotics feed on to survive. Probiotics are constantly repopulating – altering the ratio of good to bad bacteria in your gut microbiome.
There are thousands of different types of probiotics, and each is defined by its genus, species, and strain designation.
Your microbiome is comprised of diverse bacterial flora. Ideally, the balance of ‘good’ to ‘bad’ bacteria should be about 80% beneficial bacteria to 20% ‘potentially bad’ bacteria.
Remember, not everything in wheat is bad for you. There are some really good things that wheat does for us. For example, the food for the good bacteria in your gut is called prebiotics. Prebiotics keep the good bacteria fed.That’s why fiber is so important to your gut function. Prebiotics feed the probiotics (the good bacteria).
Nearly 80% of prebiotics in your diet come from wheat!
Your microbiome is sensitive to nutritional changes, and removing a commonly consumed food like wheat can have sweeping changes unless you proactively replace anticipated nutritional deficits. When you go on a gluten-free diet, you eliminate your primary source for the good bacteria in your gut (wheat).
As good bacteria gets starved of the prebiotics wheat offers, the bad bacteria continues to flourish and reproduce. This creates dysbiosis, an altered microbiome with too many bad guys and not enough good guys. You are now primed and waiting to invite disease.
With over 70% of your immune system residing in your gut, protecting those beneficial microorganisms helps to protect your overall health — including your brain health.
There are 10 times more bacteria cells in your gut than there are human cells. Bone cells, muscle cells, skin cells, organ cells — add them all up and there are still 10 times more bacterial cells than all of those cells. Those cells have 100 to 150 times more genes than the human genome. There are about 23,000 genes in the human genome, and 3,500,000 genes in the bacteria in our guts.
Genes control function. In other words, the bacteria in your gut is running the show. It tells your brain what to do. The gut isn’t your “second brain,” it’s more like the primary, and you are just the host! So, for example, if your neurotransmitters are out of balance, look to the gut. That’s where it comes from most of the time.
Research Reveals…
One study performed in 2013 examined changes in the brains of healthy women after drinking fermented milk with probiotics twice a day for four weeks. The product included four strains of probiotics: Bifidobacterium animalis subsp Lactis, Streptococcus thermophiles, Lactobacillus bulgaricus, and Lactococcus lactis subsp Lactis. Researchers concluded that this protocol affected the activity of brain regions that control central processing of emotion and sensation.
Studies continue on the use of probiotics as a viable treatment for depression and anxiety. One analysis compared probiotic consumption against depression status in over 26,000 people. While women showed no statistical improvement, “results suggest that probiotic food consumption might have beneficial effects on depression, particularly in men. Further studies are required to identify the mechanistic relations between probiotics and depression.”
People with celiac disease have a higher rate of depression. More than a third (37%) of women with celiac have symptoms of depression. Forty-nine percent of children with celiac have anxiety-related concerns. Thus, evidence suggests that if you are concerned about the health of your brain, you may want to examine your gut’s health and make improvements there first.
Your Brain Health on Gluten
A primary danger of going gluten-free is losing the food (prebiotics) feeding the good bacteria in our guts, allowing the bad bacteria to raise their numbers, and thus creating an inflammatory environment in our gut. If you are asking yourself, “If switching to a gluten-free diet can potentially cause even more inflammation, why bother?”
Let’s not find excuses for continuing something that is detrimental to your health. Let’s find solutions for restructuring and accommodating a healthier way of being.
Did you see the list of neurological and psychological problems associated with gluten-related disorders? Removing gluten from your diet can also have a positive impact when done correctly.
In an article entitled Neurologic and Psychiatric Manifestations of Celiac Disease and Gluten Sensitivity, it cites:
In 1997, a case study was published that described a woman with symptoms of schizophrenia who was diagnosed with CD following admission for her psychiatric symptoms. She presented with symptoms such as hallucinations, avolition (a lack of interest in goal-oriented behavior), and telepathic thought. She showed sluggish brain health function (slow fronto-temporal abnormalities on EEG), as well as a lack of blood flow (hypoperfusion) on the left side of her brain on SPECT scan. A gluten-free diet was administered and she showed remarkable improvement at follow-up. After just 6 months on the gluten-free diet, she no longer had hypoperfusion on SPECT scan and her psychiatric symptoms disappeared. She was even able to discontinue the use of antipsychotics, and she remained symptom-free at a 1 year follow-up.
In a review of all of the studies on schizophrenia and gluten since 1946, 66% of them showed a gluten-free diet was beneficial, often reversing the schizophrenia. The same type of thing is true with depression, anxiety, brain fog, attention deficit, autism, and many other health problems associated with the brain. When you read the science, you see that sometimes, gluten is a primary trigger causing brain dysfunction. Clearly a gluten-free diet improved her brain health, as I’ve seen in so many people who remove gluten from their diets.
These are the success stories we are aiming for.. Food can be medicine or poison. We want you to choose food that supports your brain health, gut health, and overall health.
Adding Prebiotic Foods is Essential on a Gluten-free Diet
While supplementing with prebiotics and probiotics would be wise, you can’t exclusively rely on supplements to get the job done. Your body requires real, live food, and it seems to have some preferences.
Probiotics are most effective when they are combined with a high-fiber diet that features lots of vegetables every day – nine, in fact! Vegetable fiber is critical for creating a category of compounds in our gut called short chain fatty acids (SCFA), the most famous of which is butyrate. Butyrate is the fuel for the fastest-growing cells in your body: the inside lining of your intestines. Low butyrate = high risk of colon cancer. The more diversity of vegetables in the diet, the more butyrate you produce.
So, when you go shopping for vegetables (always organic preferred), buy 1 or 2 of every root vegetable in the store. Buy rutabagas, turnips, parsnips, radish, carrot, sweet potato. Have one root vegetable every day. Then, write down a list of prebiotic foods — bananas, garlic, onion, artichoke, apples, cocoa. Eat 1 root vegetable and 2 from the prebiotic list every day.
Fermented foods can contain 100 times more probiotics than a supplement.
I recommend a forkful (or more) of fermented foods each day, varying the color and type daily. That way, you get a great variety of beneficial flora to support your immune system. Take out that fork and have some sauerkraut, or kimchi, or miso, or fermented beets, or drink some kefir or kombucha. Vary it up. If you aren’t used to fermented foods, it may take some experimentation to see which foods you tolerate well. As time goes on, your cravings may change, and you may be wanting more fermented vegetables. So stick with it!
How to Choose a Good Probiotic
Probiotic supplements help balance immune function and decrease inflammation by helping your gut maintain a stable and healthy environment. Each strain performs differently depending on your gut’s unique environment. One type of probiotic doesn’t work the same for everybody.
In general, spore-based probiotics are more effective and you get more ‘bang for your buck.’ Standard probiotics are destroyed by the hydrochloric acid in the stomach. It’s always been questioned how probiotics can work if they’re destroyed by stomach acid. Well now we know. The remnants of the bacteria destroyed in the stomach still have an inoculating benefit. These benefits are substantially better when you use spores. Remember the amber knob on the walking stick with the mosquito inside of it in the original Jurassic Park movie? That’s what spores are like — the bacteria is inside a protective casing so it’s protected from the HCl in the stomach. Thus, more of the good bacteria make their way to the large intestine and have a more profound benefit than standard probiotics.
If you want to use standard probiotics, and there’s many studies saying how beneficial it is to use them, follow the guidance of the International Scientific Association for Probiotics and Prebiotics. They recommend that you look for supplements in which the packaging contains the following information:
- Strain.
- CFUs (colony forming units).
- How many live microorganisms are in each serving?
- Expiration date, including an effective level of live bacteria through the “best by” or expiration date.
- Suggested serving size.
- Health benefits.
- Proper storage conditions (9avoid temperatures over 120 degrees).
- Corporate contact information.
Remember, you can’t out supplement your diet. Supplements are just that; they supplement. Eat the foods — the root vegetables and the prebiotics!
At first this all may seem cumbersome. I highly recommend finding a Certified Gluten-Free Practitioner or nutritionist who is well-versed in gluten-related disorders. When you have a gluten-related disorder, the treatment is a strict gluten-free diet — without exception.
Don’t let the treatment be the trigger for more problems. Take measures to protect yourself against nutritional and vitamin deficiencies associated with a gluten-free diet. Eat your vegetables (root veggies and others), every day. Without exception. You will not only protect the health of your brain, you will restore balance to your gut health and rebalance your immune system.